Research introduces new DNA methylation-based method for accurately assessing cell composition in the human pancreas, addressing a critical gap in diabetes research. By overcoming limitations of traditional protein marker-based approaches, the study provides a more precise means to identify specific cell types. The findings offer insights into beta-cell dysfunction across diabetes types and have direct clinical implications, enhancing our understanding of diabetes development and potentially guiding more tailored treatment strategies. This innovative molecular alternative to immunodetection methods holds promise for broader applications in molecular biology and diagnostics.
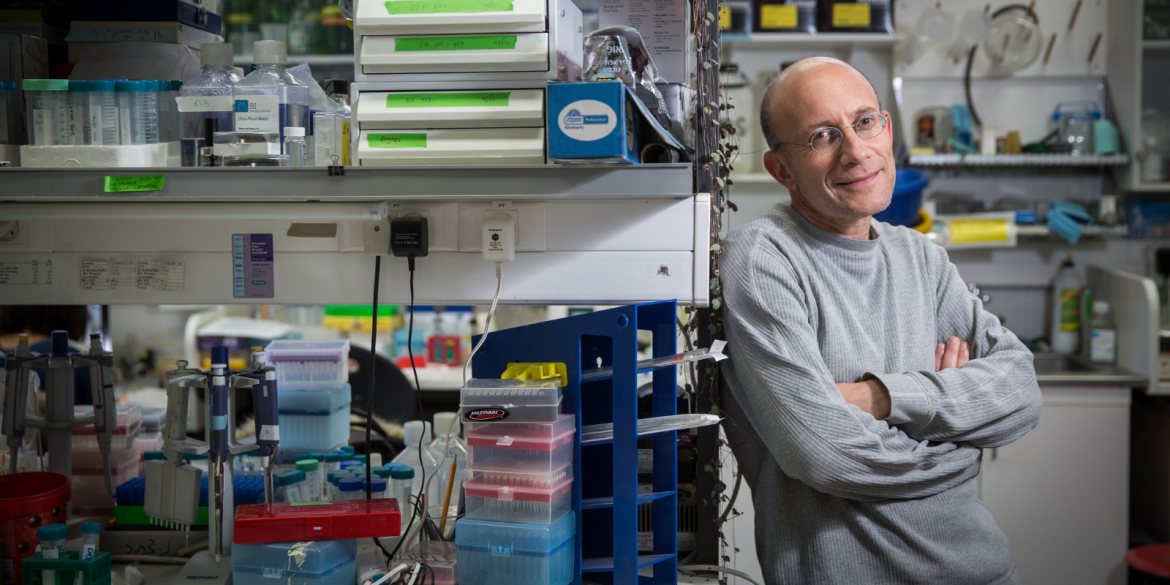
In a study published in Diabetes, Professor Yuval Dor and his research team from Hebrew University have introduced a new approach for accurately assessing cell composition in the human pancreas and islets. The research addresses a critical need in understanding the genesis of diabetes and offers an alternative to traditional protein marker-based methods.
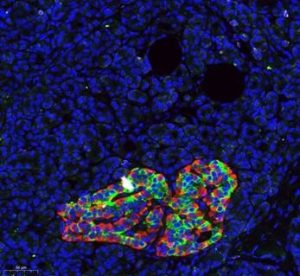
Histological image of the human pancreas, stained with antibodies against insulin (green) and glucagon (red), together marking an islet of Langerhans. Blue labels DNA, marking the nuclei of all pancreatic cells. Credit: Zeina Drawshy, Dor lab.
Current methodologies rely on the detection of protein markers, such as insulin, to identify specific cell types in the pancreas. However, the variability in protein content under different physiological and pathological conditions poses a significant limitation, complicating the accurate determination of cell numbers. The study demonstrates the innovative use of cell type-specific DNA methylation markers to overcome these limitations. By identifying genomic loci uniquely demethylated in specific pancreatic cell types, the research team applied targeted PCR to assess the methylation status of these loci in human islet and pancreas specimens. This enabled a precise inference of cell type composition, offering a molecular alternative to traditional immunodetection methods.
The researchers looked at groups of cells in the pancreas called islets. They found that in people with different types of diabetes (pre-T1D, T1D, and T2D), the function of a specific type of cell called beta-cells was similar, but it was lower compared to people without diabetes. When they looked at pancreas tissues from people with recent-onset T1D, they found that the beta-cell function was within the normal range, suggesting a problem with these cells. In people with T2D, there were more of another type of cell called alpha-cells, but the beta-cell function was normal. This helps us understand how these cells work in diabetes.
Prof. Yuval Dor, the lead researcher, remarked, “The use of DNA methylation-based analysis not only provides a more accurate assessment of cell types in the human pancreas but also proves invaluable in interpreting insulin secretion assays. This method opens new avenues for understanding pancreas cell composition in both health and disease.”
The study was led by graduate student Zeina Drawshy, Dr Agnes Klochendler and Prof. Yuval Dor from the Hebrew University, in collaboration with scientsts from Hadassah Medical Center, the University of Florida, the University of Pennsylvania and Li Ka Shing Centre for Research in Edmonton.
The study, titled “DNA methylation-based assessment of cell composition in human pancreas and islets,” has been published in Diabetes and can be accessed here.
Researchers:
Zeina Drawshy1, Daniel Neiman1, Ori Fridlich1, Ayelet Peretz0, Judith Magenheim1, Andrea V Rozo2 3, Nicolai M Doliba2 3, Doris A Stoffers2 3, Klaus H Kaestner2 3, Desmond A Schatz4, Clive Wasserfall5, Martha Campbell-Thompson5, James Shapiro 6, Tommy Kaplan1 7, Ruth Shemer1, Benjamin Glaser1, Agnes Klochendler1, Yuval Dor1
Institutions:
1) Department of Developmental Biology and Cancer Research, Institute for Medical
Research Israel-Canada, Faculty of Medicine, The Hebrew University of
Jerusalem
2) Human Pancreas Analysis Program.
3) Department of Genetics and Institute for Diabetes, Obesity, and Metabolism, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
4) Departments of Pediatrics and.
5) Pathology, Immunology, and Laboratory Medicine, University of Florida, Gainesville, FL, USA.
6) Faculty of Medicine & Dentistry – Surgery Department, 1-002 Li Ka Shing Centre for Research, Edmonton, Alberta, Canada.
7) School of Computer Science and Engineering, The Hebrew University of Jerusalem, Israel.
Disclaimer: In these challenging times of war and crisis, Hebrew University of Jerusalem is resolute in its dedication to advancing research and education. We stand in full support of the brave individuals on the frontlines, safeguarding our nation and the well-being of all Israelis, and extend our deepest gratitude and unwavering solidarity to our community and fellow citizens. Together, we shall prevail against the challenges that confront us, and our shared commitment to the well-being of all Israelis and the pursuit of knowledge remains resolute.
The Hebrew University of Jerusalem is Israel’s premier academic and research institution. With over 25,000 students from 90 countries, it is a hub for advancing scientific knowledge and holds a significant role in Israel’s civilian scientific research output, accounting for nearly 40% of it and has registered over 11,000 patents. The university’s faculty and alumni have earned eight Nobel Prizes and a Fields Medal, underscoring their contributions to ground-breaking discoveries. In the global arena, the Hebrew University ranks 86th according to the Shanghai Ranking. To learn more about the university’s academic programs, research initiatives, and achievements, visit the official website at http://new.huji.ac.il/en
